-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Trending Topics
Publication
Recycling of Large Lithium-Ion Batteries From a Property Insurance Perspective
Publication
Looks Like Inflation Is Sticking Around. What Do We Do Now? [Part 3 of 3]
Publication
The Future of Cryptography and the Rise of Quantum Computing
Publication
Personal Injury Compensation in Europe: An Updated Comparison Among Different Systems Within the European Market
Publication
How to Plan for Cat Claims - Before, During, and After an Event -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Training & Education
Publication
The Future Impacts on Mortality [Video]
Publication
Beware of Demo Mode on Electrocardiogram Reports
Publication
Understanding Breast Cancer in Asia – Awareness and the Importance of Screening
Publication
Marginal Gains in the Medicare Supplement Market U.S. Industry Events
U.S. Industry Events Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Diabetes Type 2 – Global Collaboration, Transformation, and Challenge

While we reflect upon the global epidemic of type 2 diabetes (T2DM), the journey of biomedical discovery and transformation from past to present represents inspiration, hope, and challenge.
The Discovery of Insulin: 102 years ago
It is remarkable that the earliest scientific discoveries relevant to diabetes were inspired by students in diverse global regions. In 1869, in Germany a medical student named Paul Langerhans identified the area of the pancreas found to produce insulin and named the Islets of Langerhans. 102 years ago, collaboration at the University of Toronto between a 29‑year-old Canadian surgeon, Frederick Banting, and his 22‑year-old research student, Charles Best, transformed the landscape of diabetes treatment. Best was born in Maine but attended the University of Toronto to train as a physician. In November 1921, Banting and Best’s experiments finally succeeded as they treated a diabetic dog with their insulin extract. Banting initially declined the 1923 Nobel Prize awarded to him (and Dr. J. McLeod) for this discovery as his collaborator Best had not been recognized; Banting later shared his prize with Best.
Rising Global Prevalence and Disparities
The rising global prevalence of type 2 diabetes particularly affects underserved communities and aligns with the increasing global prevalence of obesity.
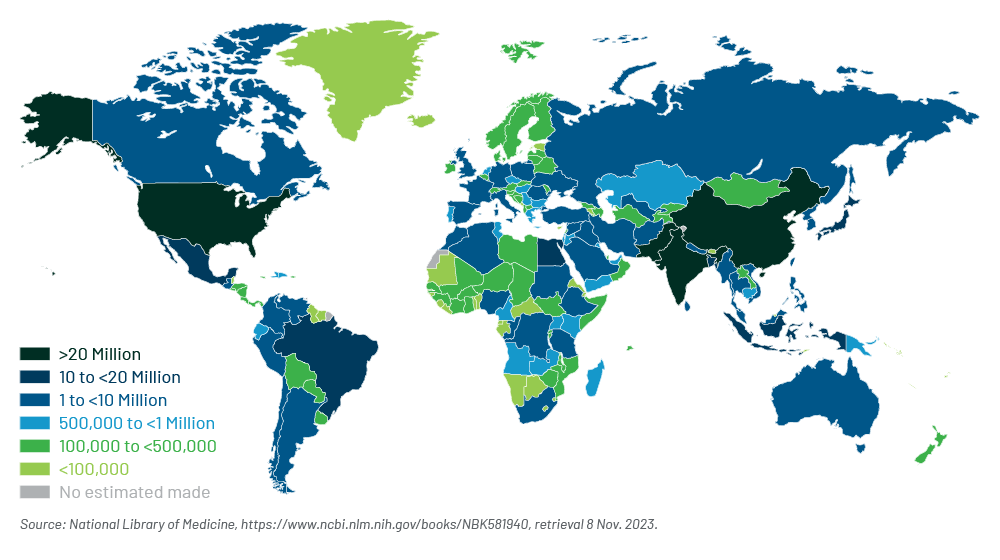
Diabetes (98% T2DM) affects 537 million adults worldwide.1
Other facts include:
- Global prevalence: 10.5% age 20‑792
- U.S. prevalence per CDC: 11.3% (37.3M; 8.7M or 23% undiagnosed)3
- Undiagnosed: Prevalence declining except in the underserved4
Estimated Total Number of Adults (ages 20‑79) With Diabetes in 2021
Global Differences and Interdisciplinary Collaboration: Asia
Understanding global differences is essential due to increasing population migration and diversity. Clinical aspects of T2DM vary in different populations and this understanding will enhance recognition of diabetes, including severity in North America.
Dr. Juliana Chan, a globally renowned diabetologist and the founder of the Asia Diabetes Foundation, has made many important contributions to diabetes research, care, and education.5 Her research identified that T2DM in the East Asian population differs from among those of European descent due to occurrence with lower body mass index (BMI), visceral adiposity with slimmer waist circumference, younger age of onset with early insulin resistance, early insulin treatment, and higher risk of complications including renal disease and cardiovascular complications.6) She led the 44‑member team of global experts in diabetes and public health that authored the 2020 “The Lancet Commission on Diabetes: Using data to transform diabetes care and patient lives”.7
Consider “Clusters of Comorbidities”
The impact of T2DM on mortality and morbidity should be considered as part of a tapestry of comorbidities including but not limited to obesity, hypertension, hyperlipidemia, cardiovascular disease, renal disease, obstructive sleep apnea, and psychiatric conditions. These comorbidities are causally interconnected and integrated assessment in medical care optimizes outcomes. Undiagnosed hyperglycemia may lead to organ damage and contribute to microvascular and macrovascular complications before T2DM is diagnosed.8
What Have we Learned?
Among the many things we have learned from more than a century of discovery are beneficial approaches to diagnosis and treatment of T2DM. Increased knowledge about T2DM has led to population screening, early diagnosis, and improved medical management and outcomes. For example, new treatments such as GLP‑1 agonists optimize diabetic control. Additionally, increasingly available are tools to optimize environmental factors such as diet and exercise via digital approaches and wearable technology. Efforts to decrease stigmatization continue as practitioners work to dispel the misperception that diabetes is caused solely by bad “habits”. This message is reinforced by knowing that diabetes is caused by complex interactions between thousands of genes and environmental factors, including prenatal factors. Global collaborations in research and education are increasing.
Despite these advancements, there is a need for ongoing vigilance in monitoring, studying, and educating people about the disease. Among the ongoing challenges are the increasing prevalence of obesity and other risk factors, such as diet, associated with the increasing prevalence of T2DM and comorbidities. The increasing prevalence of diabetes in children and adolescents aligns with the increasing incidence of childhood obesity. Ongoing disparities of access to medical care and treatment must be addressed, with particular attention to the high cost of insulin in some countries, which amplifies health risks and access disparities. More recently, in addition to the challenges presented by their high cost, off-label use of GLP‑1 agonists to treat obesity has created drug shortages for those with diabetes.
T2DM and comorbidities significantly impact population mortality, morbidity, and the economic burden on health care systems. T2DM represents a highly variable group of conditions; even with optimal management, complications and treatment challenges may occur.
What Have we Learned?
Insurers recognize the increasing need for internal and external multi-disciplinary collaboration. As part of their ongoing work in Life and Health markets, insurers should keep in mind the following forward-looking practices and suggestions regarding T2DM.
- Monitor the evolving prevalence and mortality/morbidity impact in an era of increasing underwriting acceleration
- Consider the effect of T2DM upon future Mortality Improvement Impact analyses
- Consider the population impact of innovations such as GLP‑1 agonists for weight loss
- Consider integrated “clusters” of disease (T2DM and comorbidities) for data analytics (actuarial, underwriting, and claims)
- Watch for opportunities
- New Product development targeted to diabetic applicants
- Wellness, including prevention
- Consider pricing
- Reassess current practices (e.g., Will pricing for BMI alone address the associated risk?)
- Consider risk stratification (e.g., can it be enhanced with wearables data?)
Enhancing population outcomes for diabetes will require global collaboration and ongoing public health interventions to address the challenges posed by this complex group of diseases.
Gen Re’s global experts in multiple disciplines stay informed on topics such as this, and we share the most up to date knowledge with our clients. Reach out to me if you’d like to learn more about this or another topic.
- IDF Diabetes Atlas 2021, 10th Ed, Magliano DJ, Boyko EJ; IDF Diabetes Atlas 10th edition scientific committee, Brussels: International Diabetes Federation, 2021; https://www.ncbi.nlm.nih.gov/books/NBK581940
- Ibid
- Centers for Disease Control and Prevention, National Diabetes Statistics Report, https://www.cdc.gov/diabetes/data/statistics-report/index.html?ACSTrackingID=DM72996&ACSTrackingLabel=New%20Report%20Shares%20Latest%20Diabetes%20Stats%20&deliveryName=DM72996
- National Library of Medicine, Undiagnosed Diabetes in U.S. Adults: Prevalence and Trends, https://pubmed.ncbi.nlm.nih.gov/35817030
- American Diabetes Association, Professor Juliana Chung Ngor Chan: Tireless Trailblazer for Diabetes Research, Care, and Education in Asia, https://diabetesjournals.org/care/article/45/10/2207/147654/Professor-Juliana-Chung-Ngor-Chan-Tireless
- Ann. N.Y Acad. Sci. 1281 (2013) 64-91, https://pubmed.ncbi.nlm.nih.gov/23551121/
- Lancet 2021: 396 2019-2082, https://pubmed.ncbi.nlm.nih.gov/33189186
- BMJ Open Diab Res Care 2020;8:e001549. doi:10.1136/bmjdrc-2020-001549
Some further reading on genre.com:
All endnotes last accessed on 8 November 2023.